The human spinal cord is a marvel of biological engineering, a delicate yet resilient structure that serves as the communication highway between the brain and the rest of the body. Unfortunately, like any part of the body, it can be susceptible to tumors, which can have debilitating effects on a person’s mobility and overall quality of life. Spinal cord tumors are relatively rare but can be extremely challenging to treat due to their location and complexity. However, recent advances in research and spinal cord tumor treatment modalities offer hope for improved outcomes and quality of life for patients facing this diagnosis.
Understanding Spinal Cord Tumors
Spinal cord tumors can be classified into two main categories: intramedullary and extramedullary. Intramedullary tumors originate within the spinal cord itself, while extramedullary tumors develop outside the spinal cord but within the spinal canal. These tumors can be further categorized based on their tissue type, with the most common types being gliomas, meningiomas, and nerve sheath tumors.
One of the challenges in treating spinal cord tumors is their location within the central nervous system, which can make surgical removal difficult without causing damage to surrounding healthy tissue. Additionally, the potential for neurological deficits post-surgery underscores the importance of developing less invasive treatment options that minimize collateral damage.
Advances in Imaging Techniques
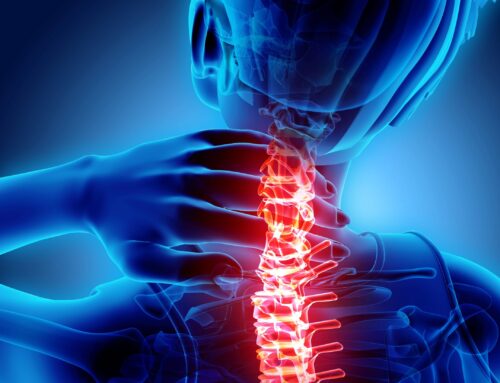
Accurate diagnosis is the first crucial step in effective spinal cord tumors treatment. Recent advances in imaging techniques have revolutionized the way these tumors are detected and characterized. High-resolution magnetic resonance imaging (MRI) combined with advanced imaging sequences allows for detailed visualization of spinal cord anatomy and the precise localization of tumors. Techniques such as diffusion tensor imaging (DTI) provide valuable information about the integrity of neural pathways, aiding in surgical planning and prognostication.
Moreover, the emergence of intraoperative MRI and intraoperative navigation systems enables spine surgeon specialists to perform more precise and complete tumor resections while minimizing the risk of damage to surrounding neural structures. These technologies have significantly improved surgical outcomes and reduced the incidence of postoperative complications.
Targeted Therapies and Immunotherapy
Traditional treatment modalities for spinal cord cancer have primarily focused on surgery, radiation therapy, and chemotherapy. While these approaches remain important components of treatment, recent years have seen a growing interest in targeted therapies and immunotherapy.
Targeted therapies involve drugs that specifically target molecular pathways involved in tumor growth and progression. For example, inhibitors of vascular endothelial growth factor (VEGF) have shown promise in the treatment of spinal cord hemangioblastomas, reducing tumor vascularity and slowing disease progression.
Immunotherapy, which harnesses the body’s immune system to target and destroy cancer cells, has also emerged as a potential treatment strategy. Checkpoint inhibitors, such as pembrolizumab and nivolumab, have demonstrated activity in certain types of spinal cord tumors by enhancing the immune response against tumor cells.
While targeted therapies and immunotherapy hold great promise, further research is needed to identify biomarkers that predict response to treatment and to optimize treatment regimens for individual patients.
Advances in Radiation Therapy
Radiation therapy plays a crucial role in the management of spinal cord tumors, either as adjuvant therapy following surgery or as a primary treatment modality for inoperable or recurrent tumors. Recent advancements in radiation therapy techniques have improved the precision and effectiveness of treatment while minimizing damage to surrounding healthy tissue.
Stereotactic radiosurgery (SRS) delivers highly focused radiation beams to the tumor site with submillimeter accuracy, sparing adjacent critical structures. This approach is particularly beneficial for small, well-defined tumors or for targeting residual tumor tissue following surgical resection.
Moreover, proton therapy, which delivers radiation using charged particles instead of traditional photons, offers the advantage of precise dose delivery with minimal exit dose, reducing the risk of radiation-induced damage to surrounding tissues. Proton therapy is especially advantageous for tumors located near critical structures such as the spinal cord, where minimizing radiation exposure is paramount.
Future Directions and Challenges
While significant progress has been made in the diagnosis and treatment of spinal cord tumors, several challenges remain. One key area of focus is the development of personalized treatment strategies based on the molecular characteristics of individual tumors. Identifying biomarkers predictive of treatment response and disease prognosis will be essential for tailoring therapy to the unique needs of each patient.
Additionally, improving access to specialized care and multidisciplinary treatment teams is crucial for optimizing patient outcomes. This includes not only access to cutting-edge treatments but also comprehensive supportive care services to address the physical, emotional, and psychosocial needs of patients and their families.
Conclusion
In conclusion, advances in spinal cord tumor research and treatment offer hope for improved outcomes and quality of life for patients facing this challenging diagnosis. By continuing to invest in research, technology, and collaborative care models, we can strive toward better treatments.