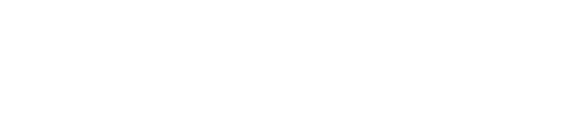
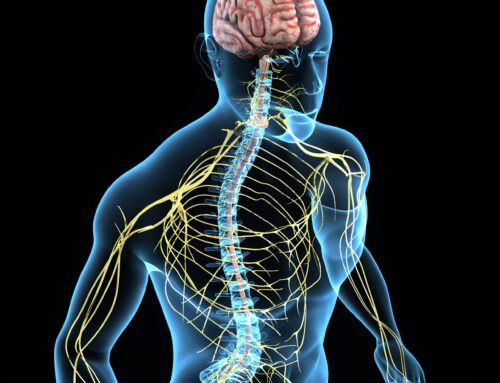
Pituitary tumors, though often noncancerous, can greatly impact a person’s health due to the important role the pituitary gland plays in regulating hormones throughout the body. Located at the base of the brain, this small gland controls various functions, including growth, metabolism, and reproduction. When a tumor develops in the pituitary gland, it can cause a wide range of symptoms, from vision problems to hormonal balance issues. Early diagnosis and effective treatment are key to managing these tumors and preventing long-term health issues.
This guide provides insight into the latest treatments available for pituitary tumors, helping patients understand their options and what to expect from the treatment process.
Types of Pituitary Tumors
Before diving into treatment options, it’s important to understand that there are different types of pituitary tumors, each of which may require a different approach. The two primary types of pituitary tumors are functioning and non-functioning tumors.
- Functioning tumors produce excess hormones, which can lead to significant hormonal imbalances. For example, a tumor that overproduces prolactin may cause reproductive issues, while those affecting growth hormones can lead to conditions like acromegaly.
- Non-functioning tumors, on the other hand, do not produce hormones but can cause symptoms by pressing on surrounding structures, including the optic nerves.
Knowing the type of pituitary tumor is essential in determining the most appropriate treatment path.
Symptoms of Pituitary Tumors
The symptoms of pituitary tumors vary widely depending on their size and whether they are functioning or non-functioning. Common symptoms may include headaches, vision disturbances (particularly loss of peripheral vision), unexplained fatigue, and hormonal imbalances that can manifest as weight changes, mood swings, or menstrual irregularities.
Patients with functioning tumors might experience symptoms related to the specific hormone being overproduced. For instance, those with Cushing’s disease, caused by excess cortisol, might have high blood pressure, weight gain, and skin changes. Understanding the symptoms is an essential step in seeking timely medical advice and receiving an accurate diagnosis.
Diagnosing Pituitary Tumors
Accurate diagnosis of pituitary tumors involves a combination of imaging, hormone testing, and physical examination. Magnetic Resonance Imaging (MRI) is the most common imaging technique used to visualize the pituitary gland and any abnormalities. It helps doctors assess the size, location, and impact of the tumor on nearby structures.
In addition to imaging, blood tests are used to measure hormone levels. Testing for specific hormone levels, such as prolactin or cortisol, if a functioning tumor is suspected, helps confirm the diagnosis. Based on these tests, a treatment plan can be developed to address both the tumor itself and any hormonal imbalances it may have caused.
Pituitary Tumors Treatment
Surgery remains one of the most common and effective treatments for pituitary tumors, especially when the tumor is causing significant symptoms or compressing nearby structures like the optic nerves. The most widely used surgical approach is transsphenoidal surgery, where the tumor is removed through the nasal passages and sinuses. This minimally invasive surgery reduces recovery time and avoids visible scarring, making it an attractive option for many patients.
In addition to transsphenoidal surgery, endoplasm surgery is emerging as a technique being explored in advanced neurosurgical procedures. Though still in the early stages of research and not yet widely implemented, it aims to enhance precision when removing tumors located near sensitive brain structures.
In cases where the tumor is larger or more complex, a craniotomy (opening the skull to access the brain) may be necessary. This approach is typically reserved for tumors that cannot be safely accessed through the transsphenoidal route. While more invasive, craniotomies allow surgeons to reach and remove difficult tumors.
Radiation Therapy for Pituitary Tumors
For patients whose tumors cannot be entirely removed through surgery or for those who are not ideal surgical candidates, radiation therapy offers an alternative or supplementary treatment. The goal of radiation is to target and shrink the tumor while preserving as much healthy tissue as possible.
Stereotactic radiosurgery is a popular form of radiation therapy for pituitary tumors. Despite its name, it does not involve surgery. Instead, it delivers highly focused beams of radiation to the tumor in one or more sessions. This precise targeting minimizes the risk of damaging surrounding structures, such as the optic nerves, making it an effective treatment option for small or residual tumors after surgery.
Other forms of radiation therapy, such as fractionated radiation, may be used when stereotactic radiosurgery is not suitable. This method involves administering smaller doses of radiation over several weeks, allowing the body time to recover between sessions.
Medical Therapy for Hormone-Secreting Tumors
For patients with functioning pituitary tumors, medical therapy is often used either in combination with surgery or as a standalone treatment to control excess hormone production. Medications vary depending on the type of hormone the tumor is producing.
Dopamine agonists like cabergoline are commonly prescribed for prolactin-secreting tumors (prolactinomas). These medications help reduce the production of prolactin and can even shrink the tumor in some cases.
Somatostatin analogs and growth hormone receptor antagonists are used to manage tumors that produce excess growth hormone, helping to control symptoms of acromegaly.
For tumors that cause Cushing’s disease, adrenal enzyme inhibitors may be prescribed to block the production of cortisol, relieving symptoms caused by excess cortisol levels.
In many cases, these medications can effectively control symptoms and reduce the need for more invasive treatments.
Monitoring and Follow-Up Care
Treating a pituitary tumor doesn’t end once the tumor is removed or reduced. Long-term follow-up care is essential to ensure that the tumor does not return and that any hormonal imbalances are properly managed. Patients will typically undergo regular MRI scans and blood tests to monitor for signs of recurrence.
For those who had functioning tumors, hormone replacement therapy may be necessary if the pituitary gland’s normal function was compromised during treatment. For example, patients may need thyroid hormone replacement, cortisol supplements, or reproductive hormone therapy to maintain a healthy balance of hormones in the body.
Additionally, ongoing collaboration between the neurosurgeon, endocrinologist, and patient is critical to ensure optimal health outcomes.
Emerging Treatments for Pituitary Tumors
Ongoing research into pituitary tumors is leading to the development of new, innovative treatments. One promising area of exploration is the use of targeted therapies, which aim to attack specific genetic mutations or proteins involved in tumor growth. These treatments have the potential to offer more precise, personalized care with fewer side effects than traditional methods.
Another exciting advancement is the use of immunotherapy, which harnesses the body’s immune system to fight tumors. While still in the early stages of research, immunotherapy shows promise in treating pituitary tumors that do not respond to conventional treatments.
Researchers are also investigating ways to improve the precision and effectiveness of radiation therapy, such as using advanced imaging techniques to better target the tumor while sparing healthy tissue.
Conclusion
Understanding the latest treatments for pituitary tumors can help patients make informed decisions about their care. Whether through surgery, radiation, or medical therapy, today’s treatment options offer a high success rate in managing these tumors and improving patients’ quality of life. As medical research continues to evolve, patients can look forward to even more effective and less invasive treatment options in the future. Regular monitoring and collaboration with a specialized medical team will ensure the best outcomes for individuals affected by pituitary tumors.